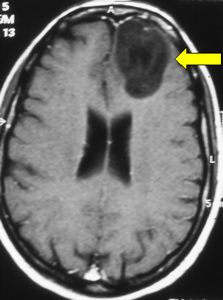
Fig.4.1: This MRI image shows a typical left frontal low-grade astrocytoma (arrow), whose presenting symptom is epilepsy.
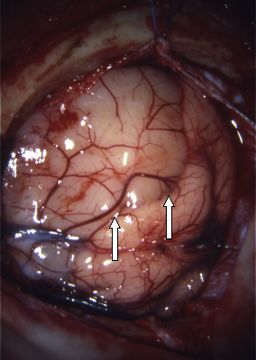
Fig.4.2: Operative view of the same tumor (arrows), whose color is different from the one of normal brain.
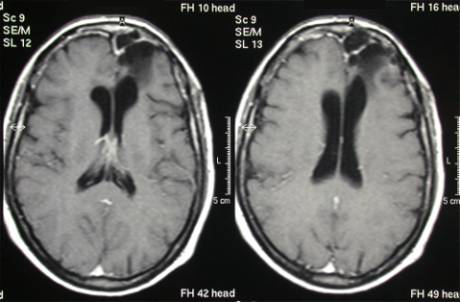
Fig.4.3: Same case, 6 years after radical surgery.
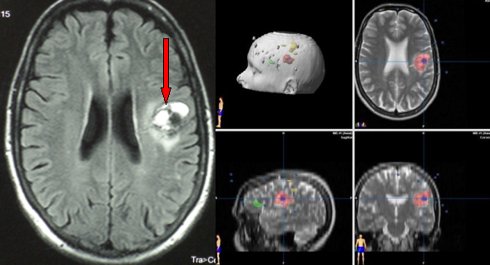
Fig.4.4: Typical appearance of a cavernous angioma (cavernoma) at MRI (red arrow), whose presenting symptoms often include seizures. On the right, planning of the surgery with the neuronavigator; the green area is the language one, the yellow the motor one.
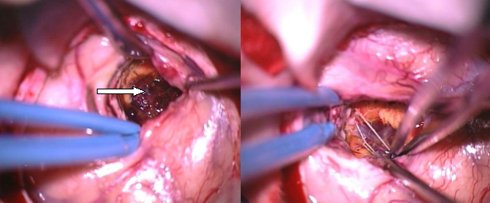
Fig.4.5: View under the operating microscope. The lesion is indicated by the arrow. On the right, the brain after removal of the cavernoma.
An epileptic seizure is an attack due to abnormal electrical activity of the brain; it may cause abnormal movements. If it is generalized, it is accompanied by loss of consciousness.
There are different kinds of seizures, depending on the affected area of the brain (in our cases, on the location of the brain tumor).
Seizures occur suddenly, without an apparent reason. Sometimes, the person feels a strange sensation before the crisis, which may be gastric, visual or psychic. This sensation is called "aura". It is generally constant in the person involved.
Generalized Seizures
There is loss of consciousness. The person falls without trying to protect him/herself. The person does not remember his/her crisis. A generalized crisis may follow a partial one.
The typical crisis, as described in novels and movies, is the "grand mal" crisis. The person falls, has tonic-clonic tremors, temporary respiratory arrest, closes his/her mouth firmly, loses urine and his/her pupils are dilated. The attack lasts 1-2 minutes. It is an impressive event, but less severe than it may appear. It stops by itself, does not need medical assistance (unless repeated). A pillow under the head is useful. In case of vomiting, the lateral position is important. After the crisis, there is generally some drowsiness and severe headache, due to cerebral edema.
Partial Seizures
They may be motor or sensory. They start from a limb and may then extend to the rest of that side of the body. The movement is rhythmic and may last for some minutes, after which the limbs may remain weak for some time. This kind of epilepsy is called Jacksonian. Sensory Jacksonian epilepsy is characterized by a strange sensation starting from a limb and then extending to that half of the body.
Partial seizures may be also psychic, visual or olfactory, depending on the brain area where they initiate.
Post-Surgical Epilepsy
After neurosurgery, some patients may develop seizures due to their recent scar and/or residual brain tumor. Thus, antiepileptic drugs are generally given to these patients for some months, sometimes on a life-long basis. For those that have developed seizures pre- and/or post-operatively, this is a good indication.
No studies have demonstrated the efficacy and usefulness of preventive antiepileptic drugs in patients who have been operated for brain tumor and never experienced seizures. Some antiepileptic drugs, mainly barbiturates, negatively interfere with chemotherapy. Consequently, they should not be given to patients with malignant tumors that may be eligible for chemotherapy. Well-organized neurosurgical departments have neurologists that are dedicated to the treatment of brain tumor-associated seizures.
Pagina 10



 General Symptoms
General Symptoms Previous Page
Previous Page