SPINAL AND PERIPHERAL NERVE NEUROSURGERY
Many operations of spinal surgery are performed at the Neurosurgical Division of the "Regina Elena" National Cancer Institute.
For intradural spinal cord tumors: (glioma, ependymoma, hemangioblastoma, meningioma, neurinoma or neurofibroma) see Chapters 5 and Chapters 7.
The tumors of the spine may be primary or, much more frequently, metastases from tumors located in other sites: prostate, breast, lung, hematological malignancies.
Primary tumors are osteomas, chondromas and chordomas. These are slow- growing lesions that present with pain, sometimes very severe pain, and that may compress the spinal cord and the spinal nerves. The malignant types of the primary tumors of the spine are the rarest.
Metastatic spinal tumors may be of neurosurgical interest, in that they require palliative surgery for severe pain and/or neurological deficit. Obviously, the symptomatic lesion must be single, i.e. the rest of the spine should be fairly healthy and the patient's life expectancy should be so long as to allow a reasonable period of good quality of life. Chemo-radiotherapy must also be available.
Surgery must be performed in specialized centers, where stabilization of the spine can be done at the same time.
Injection of a synthetic cement, Polymethylmetacrylate (PMMA), into the affected body of the vertebra, through the pedicle, is called vertebroplasty. This is a straightforward and quite safe way to stabilize the metastatic spine. It can be done on more segments in same session. Good results are achieved in terms of pain relief. Not all the vertebral bodies are suitable for this technique, as the PMMA must not escape into the spinal canal. The walls of the body should be intact.
PMMA injection is also used for traumatic and osteoporotic fractures.
This procedure is conducted when soft metastatic tissue invades the spinal canal and compresses the cord and the nerves. The posterior part of the involved vertebras is removed and the dural sac is decompressed. Where necessary, posterior stabilization can be done, either in the same session or at a later stage.
Laminectomy is an easy-to-perform, palliative operation, which may yield very good results in terms of neurological recovery. Complete paraplegia may improve, if laminectomy is performed on an emergency basis, within 24 hours from onset of the symptoms.
Peripheral nerve tumors are neurinomas (neurofibroma, schwannoma). They may grow from any peripheral nerve. They are small, round or ovoid, hard masses that cause severe irradiating pain. The pain irradiates along the course of the nerve. Diagnosis is done with echography and/or functional MRI. It is very important to distinguish peripheral nerve neurinomas from other tumors: fibromas, lipomas and so on. This distinction is mandatory, since surgical treatment by a general surgeon, without the operating microscope, may result into a disaster. The nervous fascicles must be identified and spared. This is rather easy in skilled hands under the operating microscope.
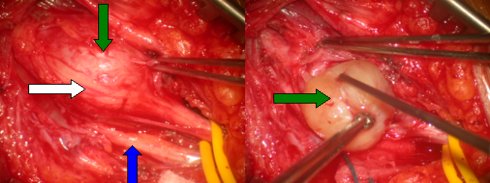
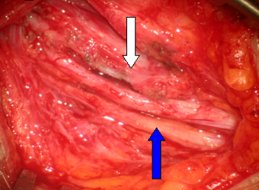
Fig.8.1: Intra-operative view of neurofibroma of the median nerve, just distal from the axilla. Above left, the green arrow points to the neurinoma; the blue one to the ulnar nerve; the white one to the healthy fibers of the median nerve. Above right, removal of the tumor (diameter: 2 cm). Below, the healthy median nerve (white arrow) and the ulnar nerve (blue arrow).
Spinal Meningioma, Spinal Neurinoma, and Spinal Hemangioblastoma paragraphes from Chapters 5
Spinal meningiomas are rather rare. They are prevalent in females. Unlike spinal gliomas or ependymomas, they grow inside the dura but outside the spinal cord, which is compressed and displaced. They present with spinal pain and progressive neurological deficit below the level of the tumor. Symptoms may be severe; the spinal canal is a narrow space and the compensation is less easy than in brain meningiomas. MRI is the most useful diagnostic tool.
Fig.8.2: Lateral MRI view of a meningioma of the 5th dorsal segment (arrow) that compresses the spinal cord.
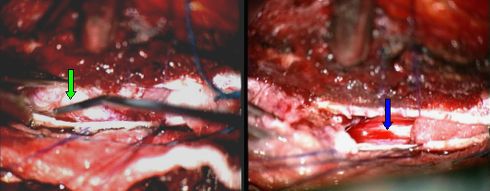
Fig.8.3: Operative view of the same case as in Fig. 5.37. The tumor (2.5 cm) is exposed (green arrow) through a "mini" window in the spine. On the right, the spinal cord after meningioma removal (blue arrow).
They are benign tumors, similar to their intracranial counterparts. They are a little bit different in histology and may be called neurofibromas. They grow from the nerves within the spinal dura and outside the spinal cord: intradural extramedullary tumors. At times, they follow the nerve outside the spine in a dumbbell shape. They may be multiple. The most frequent location is in the lumbar spine, i.e. the neurofibroma takes origin from one of the nerves of the cauda equina.
Pain is the most frequent symptom; nocturnal pain, relieved in the upright position, is typical. If the spinal cord is compressed, there may be paraparesis or other senso-motor deficits, depending on the level of the lesion. Sphincteric disturbances may be present in large caudal neurofibromas.
Contrast-enhanced MRI is the tool for the diagnosis of spinal neurinomas.
The only therapy is microneurosurgical removal. Like in spinal meningioma, the mininvasive approach is relatively easy in experienced hands. Mininvasive neurosurgery shortens hospital stay, lowers costs, lessens the use of post-operative medication and abolishes the use of post-operative external devices and the risk of late spinal instability.

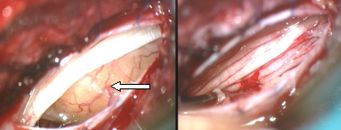
Fig.8.3: On the left, MRI picture of a spinal neurofibroma at L1 (red arrow); the yellow arrow points to the spinal cord. In the center, the tumor as seen under the operating microscope, through a mininvasive approach; on the right, the "cauda equina" after tumor removal.
Cerebellar hemangioblastomas present with gait disturbances, hydrocephalus and intracranial hypertension. Spinal cord hemangioblastomas present with slow-worsening paraparesis or tetraparesis.
The diagnosis with MRI is quite easy as their picture is typical. In the spinal cord, selective angiography may be indicated before surgery.
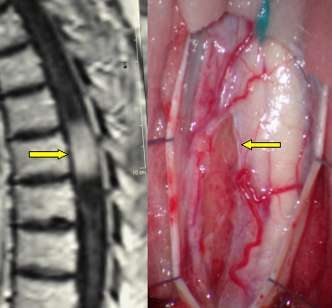
Fig. 8.5: Lateral view of MRI displaying a dorsal hemangioblastoma of the spinal cord. On the right, the incised cord under the operating microscope and the tumor that is pointed by the arrow.

Fig. 8.6: This is the operative view of the spinal cord after removal of the tumor.
Page 30



 Spinal Tumors
Spinal Tumors Previous Page
Previous Page