Epidermoids may also develop in the spinal cord.
They may be mixed with other tissues: dermoid, theratoma.
Symptoms depend on the size and location of the cyst. Both at CT scan and functional MRI, the features of epidermoids are very typical; therefore, diagnostic confusion is rare.
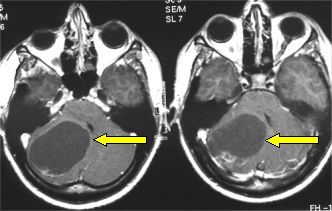
Fig.5.45: Typical MRI features of an epidermoid located in the right cerebello-pontine angle (arrow).
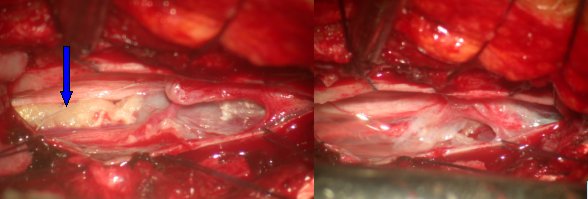
Fig.5.46: Epidermoid of the conus medullaris, as seen under the operating microscope after a mininvasive approach. On the left, the lesion pointed by the blue arrow; on the right, the conus and the cauda equina after removal.
Angiomas are malformations which are classified on the basis of the extent of their blood flow and the type of blood flowing into them.
High-flow angiomas or arterio-venous malformations (AVM) consist of a thick net of dilated arteries and veins with high flow inside them. They present with seizures, sometimes with a severe hemorrhagic event. Rupture of an AVM may cause sudden death in young people.
Diagnosis is made at MRI and Digital Angiography.
For therapy, the role of neuroradiologists is crucial, if they are able to embolize the AVM. In this way, the AVM may be cured or the work of the surgeon may be significantly facilitated, as the blood flow in the AVM is considerably reduced.
In superficial AVMs, removal may be fairly easy. For deep-seated AVM operations, a very experienced vascular neurosurgeon is needed. For small AVMs, radiosurgery may be an effective alternative to surgery.
Indications to surgery depend on symptoms: severe seizures, risk of bleeding and age of the patient. Young patients are more suitable as their life expectancy is longer and their risk of hemorrhage/year higher.
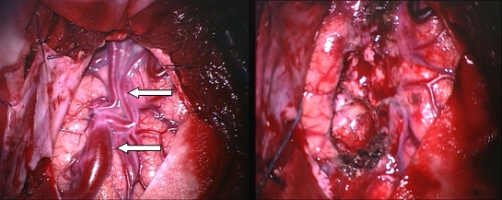
Fig.5.47a: Operative view of a superficial left temporal AVM. On the right, the bed after removal of the pathological vessels.
A second type of frequent vascular malformation or angioma is the cavernoma or cavernous angioma. Although their flow is slow or practically still, cavernomas may bleed. They are grape- or berry-shaped and may present with seizures.
Diagnosis is quite easy with MRI. CT scan and angiography are generally non-diagnostic for cavernomas.
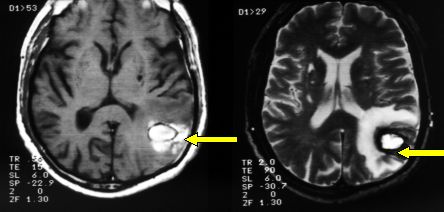
Fig.5.47: Left parietal cavernoma after recent bleeding
Microneurosurgery with careful planning via functional MRI and neuronavigator is the only therapy for cavernomas. It is indicated when the risk of bleeding is high (young people), seizures are uncontrolled with medication and their location is not very deep and/or difficult to reach. See Figs. 4.4 and 4.5.
Other angiomas (capillary, venous) are rare and usually clinically irrelevant; sometimes, they may give rise to seizures.
Page 22



 Glioma
Glioma Previous Page
Previous Page