An external device, i.e. stereotactic frame, is applied to the skull. Then, the anatomical data collected by CT Scanning, while the patient has the frame on, are processed and a target is chosen using the three spatial coordinates: x, y, and z.
Stereotactic neurosurgery is mostly used for functional neurosurgery: Parkinson's disease, other movement disorders and so on.
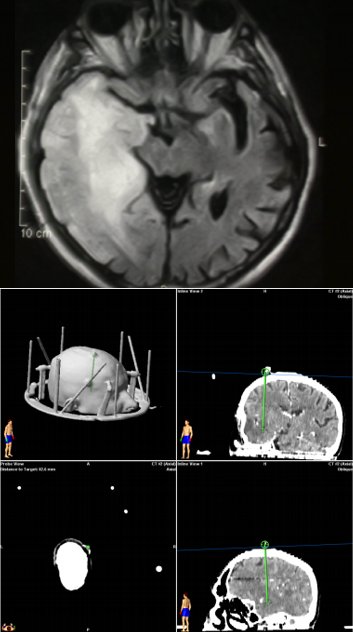
Fig.6.8: Left, MRI of a diffuse deep right temporal lesion (glioma) not suitable for open neurosurgery. Right, imaging of the stereotactic biopsy procedure, supported by the neuronavigator and by the CT Scan-calculated coordinates.
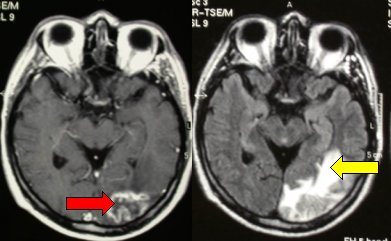
Fig.6.9: Radionecrosis after radiosurgery for kidney cancer brain metastases, as seen in different MRI scans. The red arrow shows the necrotic part of the brain, the yellow the surrounding brain edema.
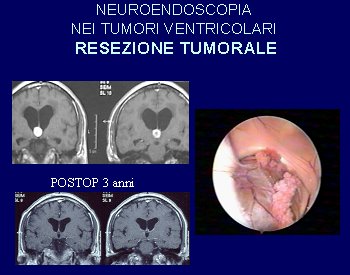
Fig.6.10: 3rd ventricle colloid cyst (top) that has been removed endoscopically; on the right, intra-operative view. On the bottom, MRI images taken after 3 years.
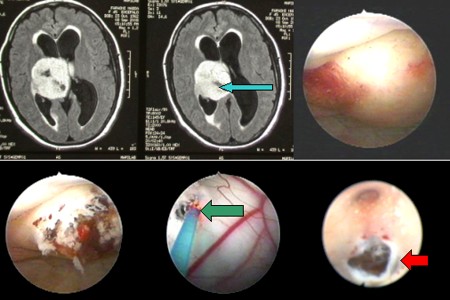
Fig.6.11: Top left, the blue arrow points to a large intraventricular brain tumor at axial MRI. Right, endoscopic view of the tumor. Bottom left, the tumor after biopsy. Bottom right, a communication is created between the ventricles to allow the CSF to flow. This is done with a laser.
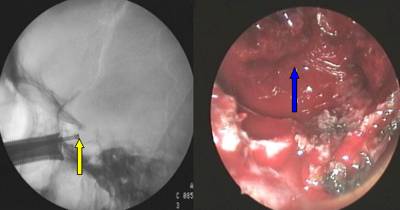
Fig.6.12: On the left, direct transnasal approach to a pituitary adenoma; the instrument enters through the nostril and reaches the anterior wall of the sella turcica (yellow arrow). On the right, endoscopic appearance of the pituitary adenoma (blue arrow) as seen with the angled endoscope, very useful to explore the hidden parts of the cavity.

Fig.6.13: Same case as in Fig. 6.7: the endoscopic view is matched with the data from the neuronavigator.
It must be kept in mind that the surgical laser is a non-invasive instrument, which is applied directly on the skin and then does the miracle.
This is a daily instrument in use for brain tumor neurosurgery, maybe the most important one introduced in the last 20 years. It permits to demolish the pathological tissue and aspirate it without traction on the surrounding tissues or vessels. It is mandatory in neurosurgery either for brain tumors or for spinal cord tumors.
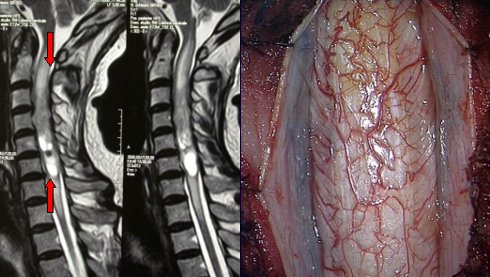
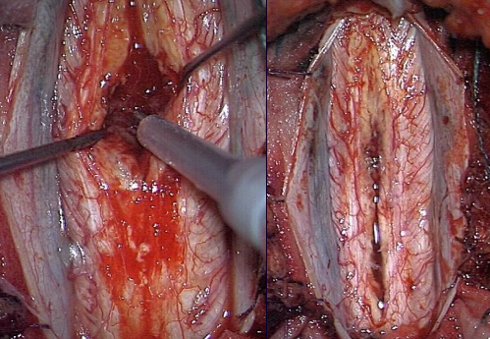
Fig.6.14: Above left, MRI of a cervical intramedullary ependymoma (red arrows). Above right, the swollen cervical cord under the operating microscope. Bottom left, the tumor is being removed with the ultrasonic aspirator (yellow arrow); right, the spinal cord after radical removal of the tumor.
Page 27



 Operating Microscope
Operating Microscope Previous Page
Previous Page